Introduction
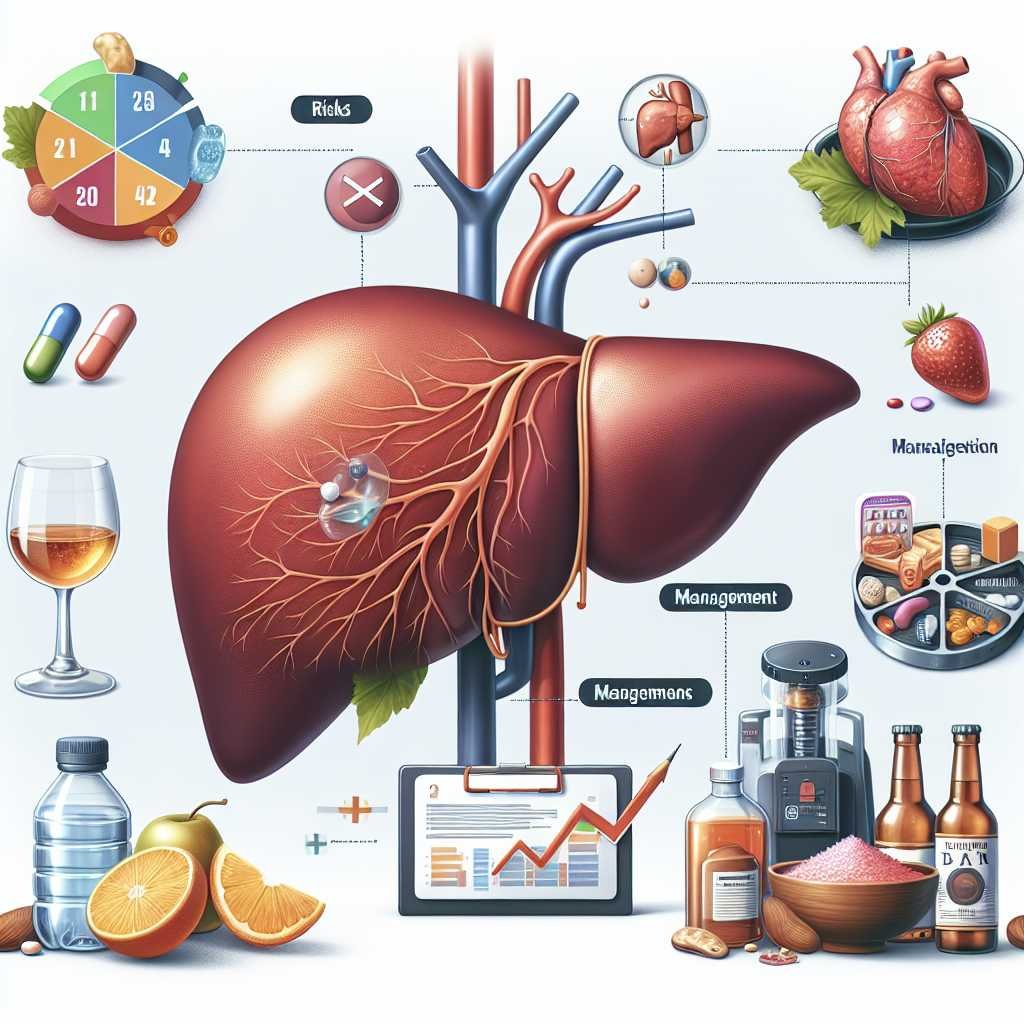
Cirrhosis is a serious liver condition characterized by severe scarring and irreversible damage to the liver. While often associated with alcohol-related liver disease, cirrhosis can arise from various liver disorders. Understanding this condition is crucial for effective management and prevention of complications.
What is Cirrhosis?
Cirrhosis occurs when the liver sustains significant damage, leading to fibrosis, which is the formation of scar tissue. While fibrosis can be reversible in its early stages, there comes a point where the liver’s ability to heal itself diminishes. Unfortunately, there is currently no cure for cirrhosis. However, addressing the underlying causes can help prevent further deterioration and liver failure.
Effective management of cirrhosis often involves symptom control and lifestyle modifications. Patients are advised to avoid substances that can exacerbate liver damage, such as alcohol, certain medications, and high-fat foods. In severe cases, a liver transplant may be necessary.
Risks and Complications
Individuals with cirrhosis face a heightened risk of developing liver cancer. Regular surveillance for liver cancer is essential, as most patients diagnosed with this condition also exhibit signs of cirrhosis. In many cases, discussions about liver transplantation arise only after significant liver damage has occurred.
Understanding Liver Functionality
It is important to differentiate between liver function and disease progression. The liver is remarkably resilient and can continue to function even when severely scarred. Consequently, some individuals may not exhibit symptoms or show elevated liver enzyme levels despite having significant liver damage. Regular consultations with healthcare providers are vital for assessing liver health and determining the need for imaging tests.
Types of Cirrhosis
Cirrhosis is generally classified into two categories: compensated and decompensated. Patients with compensated cirrhosis may not exhibit noticeable symptoms, while those with decompensated cirrhosis often feel unwell due to the liver’s compromised functionality.
Impact on Liver Structure
In cirrhosis, the liver shrinks and hardens, impairing its ability to process blood effectively. The liver receives blood from two primary sources: the hepatic artery, which supplies oxygen-rich blood, and the hepatic portal vein, which carries nutrient-rich blood from the digestive system.
Portal Hypertension and Its Consequences
In cases of decompensated cirrhosis, scar tissue obstructs blood flow through the portal vein, leading to a condition known as portal hypertension. This increased pressure can result in various complications, including varices, ascites, and hepatic encephalopathy.
Ascites
Ascites is characterized by the accumulation of fluid in the abdominal cavity due to portal hypertension. This condition can cause discomfort, swelling, and pain. In severe cases, ascites may become infected, posing a significant risk to kidney function and overall health.

Hepatic Encephalopathy
Ammonia, a byproduct of protein digestion, is typically processed by the liver and converted into urea for excretion. However, in cirrhosis, ammonia can accumulate in the bloodstream, leading to hepatic encephalopathy. Symptoms may include confusion, disorientation, and, in severe cases, coma. Management often involves medications that help reduce ammonia levels.
Kidney Complications
The liver and kidneys work in tandem to eliminate waste from the body. In cirrhosis, patients may develop hepatorenal syndrome, a serious complication characterized by progressive kidney failure.
Bilirubin and Jaundice
Bilirubin, a yellow pigment produced during the breakdown of red blood cells, is processed by a healthy liver. When liver function is impaired, bilirubin can accumulate, leading to jaundice, which manifests as yellowing of the skin and eyes. This condition can also cause dark urine and pale stools.
Varices and Their Risks
When blood flow through the portal vein is obstructed, it seeks alternative pathways, often resulting in the formation of varices—enlarged veins in the stomach and esophagus. These veins are at risk of rupturing, which can lead to life-threatening bleeding. Regular endoscopic examinations are crucial for monitoring varices and preventing complications.
Conclusion
Cirrhosis is a complex condition that requires careful management and monitoring. Understanding its implications, risks, and treatment options is essential for patients and healthcare providers alike. Regular check-ups and lifestyle modifications can significantly impact the quality of life for those living with cirrhosis.
For more information on managing specific complications related to cirrhosis, please refer to our dedicated pages on ascites, hepatic encephalopathy, and hepatorenal syndrome.

