Insight
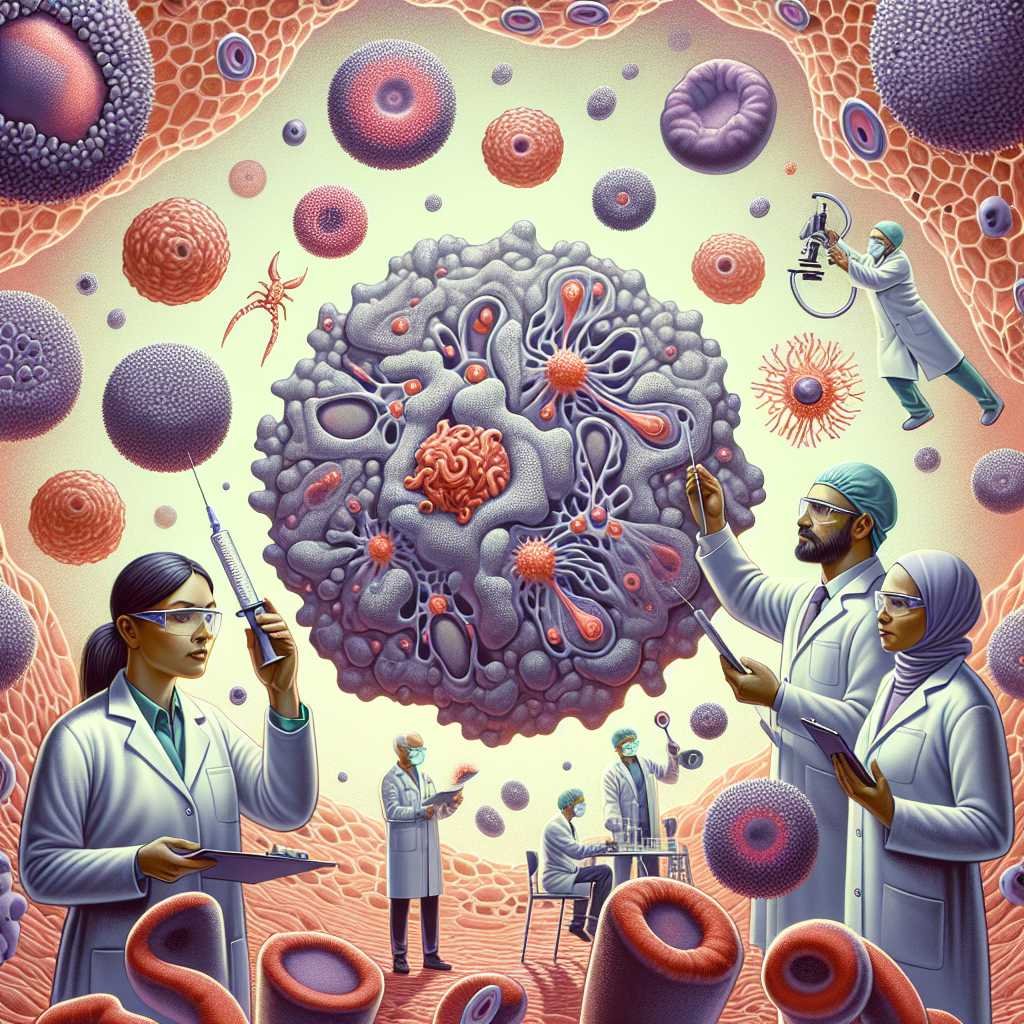
- Noncancerous cells and their soluble factors play an important role in resistance to immunotherapy.
- The composition and activity of tumor microenvironment (TME) can be used as targets of therapies.
CD19 T cells with chimeric antigen receptor (CAR) therapy has revolutionized the treatment of the most severe and refractory cases of lymphoma, but more than half of all patients have no long-term benefit from this therapy.Several studies suggest that the TME plays a central role in the mechanisms in case of failure of immunotherapy. This topic was discussed in a session at the ASH Annual Meeting_-2022, which highlighted recent advances in characterizing the microenvironment of lymphoma and its association with resistance to CAR T-cell therapy.
Ecotypes and stromal cells
Lymphoid tissue has a very rich cell diversity, with all cell types crosstalk with each other. Lymphoma embraces the microenvironment, which loses its architecture, and settles in a niche that provides survival-promoting signals and favors immune evasion. The different components of the tumor microenvironment appear to be composed of stereotyped patterns occurring with relative frequency, called “ecotypes”.
Maher Gandhi, Director of the Mater Research Institute (Brisbane, Australia), presented some recent work showing that ecotypes are associated with patient outcomes and can be subjected to therapeutic modulation.”Lymphoma ecotypes, i.e., the behavior of tumor cells prior to therapy, are likely to influence behavior after cellular immunotherapy,” he said. “New technologies such as sc-RNA-Seq and spatial transcriptomics applied to TME can help us rationalize cellular immunotherapies with small molecules, antibodies or gene modifications.”
The most abundant cells in the stromal microenvironment are cancer-associated fibroblasts (CAFs). CAFs develop together with the lymphoma cells: while the fibroblasts exhibit tumor-suppressing activities (which act as a checkpoint for lymphoma proliferation), completely reprogrammed nbsps; CAFs support tumor cells. Leandro Cerchietti of Weill Cornell Medicine (New York) presented data from his group showing that the protein HSF1 in lymphoma is crucial for maintaining the protumoral CAF phenotype and that CAF reprogramming is modified by aging and treatment pressure.”There are two ways to target the stroma in lymphoma: restoring checkpoints in the microenvironment or eliminating CAFs,” he suggested while presenting the preclinical data with hypomethylating agents and FGFR1 inhibitors. “In the future, we will likely combine therapeutic strategies targeting CAFs and lymphoma cells to improve immunotherapy, especially cell therapy.”
Immune cells and cytokines
What favors certain ecotypes and how they change when we initiate therapies with CAR-T cells or other immunomodulatory agents is not clear, but certain cell types and their activity are involved in CAR-T resistance. Frederick Locke, director of the Cellular Immunotherapy Program at Moffitt Cancer Center (Tampa, FL), describes how suppressive myeloid cells influence resistance to CAR T-cell therapy and toxicity in non-Hodgkin’s lymphoma. “Systemic inflammation is associated with reduced efficacy of CAR-T in large B-cell lymphoma,” he explained.”Tumor inflammation characterized by interferon-response genes leads to increased expression of checkpoint ligands, infiltration of suppressive myeloid cells, and increased numbers of circulating myeloid suppressor cells. These features prevent the expansion and efficacy of the CAR-T cells.”
Saad Kenderian of the Mayo Clinic (Rochester, MN) further described strategies for inhibiting suppressive myeloid cells. In preclinical models, inhibition of the GM-CSF axis improved the efficacy of CAR-T cell therapy and prevented its toxicity. The Phase I/II ZUMA-19 study demonstrated the safety of the combination of CD19 CAR T cells and a monoclonal antibody against human GM-CSF in large B-cell lymphoma. “Using several independent models, we identified IL-4 as a key regulator of CAR-T cell function,” he recently reported. “IL-4 induces a state of CAR T-cell dysfunction characterized by a transcriptional signature of fatigue.” This cytokine could be another target for improving the effectiveness of immunotherapy.
This full text is unfortunately reserved for medical professionals
You have reached the maximum number of articles for unregistered visitors
Source – https://www.univadis.de/viewarticle/ash2022-neue-einblicke-in-lymphom-mikroumgebung-ebnen-weg-fur-effektivere-immuntherapie