- In a world-first application of CAR T cell therapy, base-edited T cells were administered for the first time to a patient with relapsed T-cell leukemia.
- For gene editing, a base editing approach was used to prevent the DNA damage that occurs with other gene-editing methods.
A patient with relapsed T-cell leukemia was successfully treated with CAR-T cell therapy.
13-year-old Alyssa from Leicester (UK) was diagnosed with acute lymphoblastic T-cell leukaemia (T-ALL) in 2021.She has been treated with all current conventional therapies, including chemotherapy and bone marrow transplantation – without success.
She was the first patient to be enrolled in the TvT clinical trial, and in May 2022 she was enrolled in the Bone Marrow Transplant (BMT) Unit at Great Ormond Street Hospital (GOSH, London) to receive CAR-T cells. These came from a healthy volunteer and underwent base editing using a new technology developed by a team of researchers from the UCL was developed under the direction of Waseem Qasim (UCL Great Ormond Street Institute of Child Health). A chimeric antigen receptor (CAR) should enable the destruction of malignant T cells.
According to 28 Days the patient was in remission and received a second bone marrow transplant to restore her immune system. Now, six months after the transplant, she is at home with her family and doing well.
The researchers presented the data at the annual meeting of the American Society of Haematology in New Orleans, USA.
The use of genome-edited T cells (CAR-T cells) was first used to treat B-cell leukemia in 2015 by the same team from GOSH and University College London Great Ormond Street Institute of Child Health (UCL GOS ICH), which also recently reported studies on the use of CRISPR/Cas9 techniques in children.
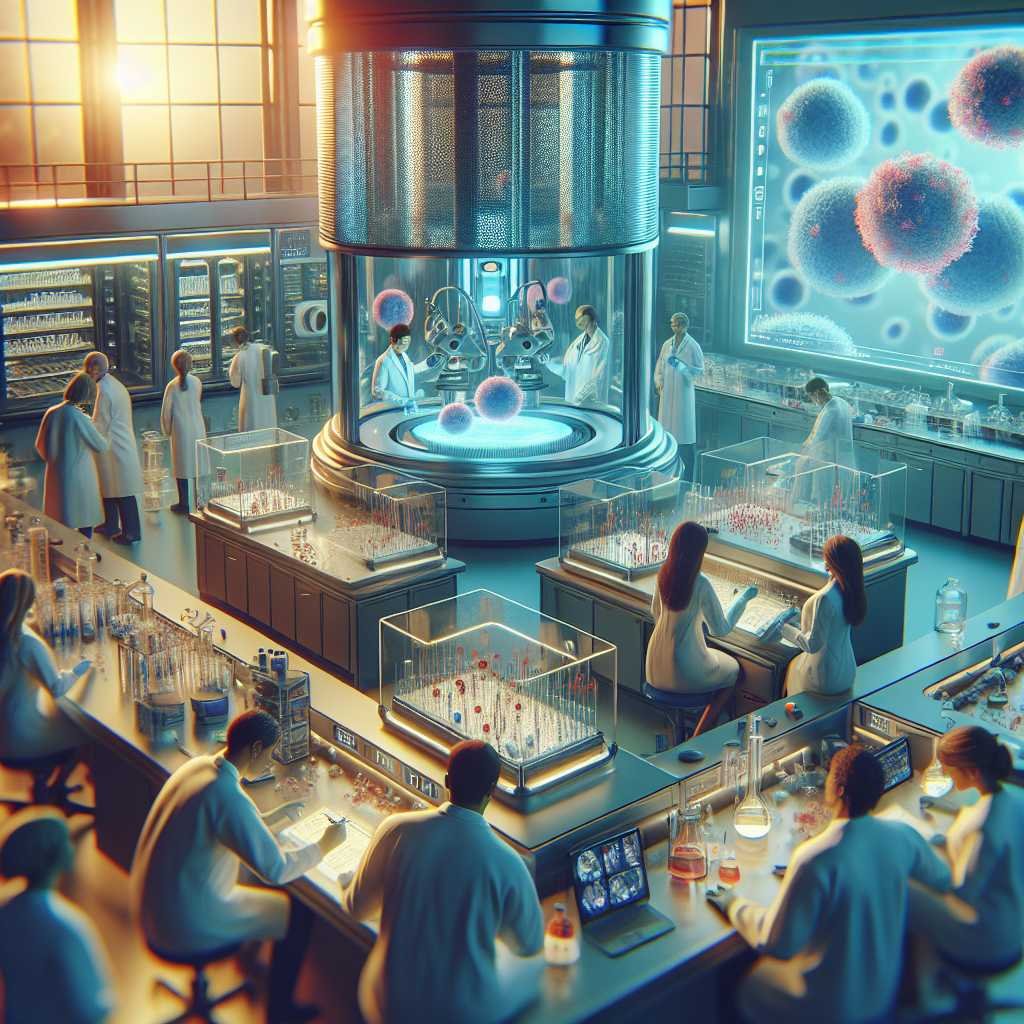
Until now, it has been difficult to treat other types of leukemia with this approach because the manipulated T cells attack each other during the manufacturing process in the laboratory. Several additional DNA edits were necessary to generate banks of “universal” anti-T cell CAR T cells for this study.
To generate these cells, healthy donor T cells were developed to which four separate modifications were made:
These changes were achieved by base editing – for example, by exchanging cytosine for thymine at a specific position in the CD7 gene to create a “stop codon”. This prevents the cell machinery from reading the full instructions, and the production of CD7 is stopped.
These gene-edited CAR-T cells are directed against the T cells in the patient’s body, including leukemic T cells. If the therapy is successful, the patient will subsequently receive a bone marrow transplant to restore the decimated immune system.
Unlike other editing techniques such as TALENS or CRISPR/Cas9, the new approach to base editing works without causing breaks in DNA. This allows for more edits with fewer risks of adverse effects on chromosomes. The technique is also being investigated to correct disease-causing changes in the DNA code in various hereditary diseases.
This full text is unfortunately reserved for medical professionals
You have reached the maximum number of articles for unregistered visitors
Source – https://www.univadis.de/viewarticle/ash2023-die-wissenschaft-hinter-der-ersten-car-t-zell-therapie-gegen-t-all